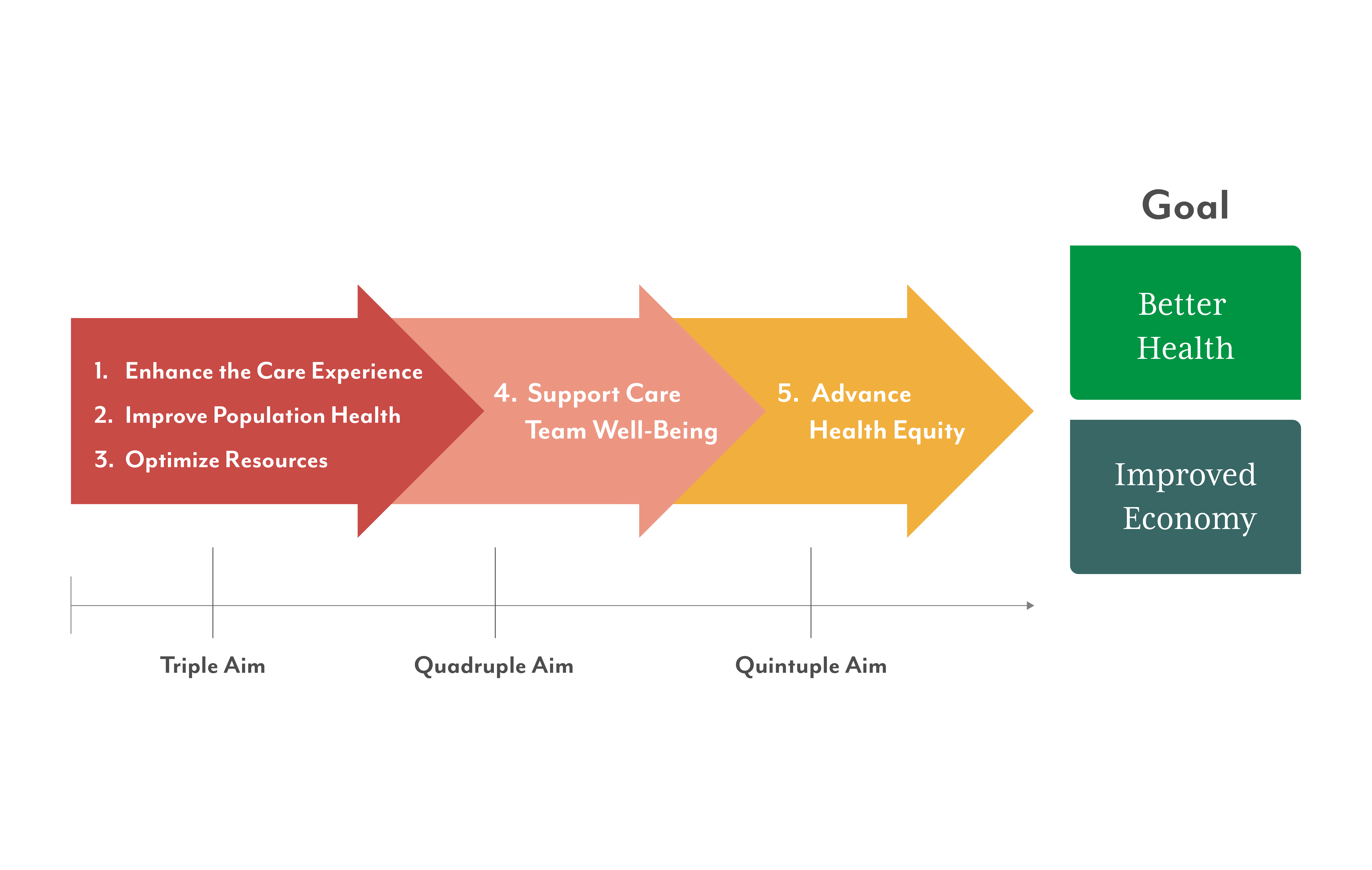
Fifteen years ago, the triple aim was introduced. Seven years later, a fourth aim was added. Today, advocates are arguing for the quintuple aim in healthcare. Is five the charm?
History of the triple aim
In October 2007, researchers at the Institute for Healthcare Improvement (IHI) proposed the triple aim, three organizing principles designed to help healthcare organizations optimize performance. The hope was that by simultaneously focusing on improved population health and enhancing the patient experience while reducing total cost of care, the healthcare system would be transformed. Shortly thereafter, the triple aim was incorporated into the national strategy for addressing healthcare issues via the Patient Protection and Affordable Care Act of 2010.
Broadly speaking, the three aims were:
- Population health: With the primary care physician (PCP) at the center, this aim focused on preventive medicine and patient education to reduce chronic disease and acute care needs (thereby reducing demands on a strained hospital system). A broad adoption of early health screenings and a robust investment in data analytics and technology would be needed to improve the health of entire populations (compared to the previous system’s individual approach).
- Patient experience: This aim strove to improve the level of service and attention people received when they did require care and advocated for including the person's point of view when developing treatment plans. The hope was that simple improvements like minimizing wait times or adopting a focus on holistic health, along with more empathetic communication, could overcome the concerns of individuals resistant to seeking care and reinforce behaviors that supported annual wellness visits. Additionally, the more people understood and participated in the creation of their individual care plans, the more likely they were to adhere to the plan, thereby improving outcomes.
- Improved value (originally conveyed as cost per capita): It’s been well-documented that the United States spends more on medical care per person than any other country,1 yet overall healthcare performance is often below the standards achieved by other national healthcare systems. The objective of this aim was to improve quality of care while simultaneously reducing the total cost of care per person.2 Changing behaviors – like earlier and better health screenings, reducing inappropriate use of emergency rooms and providing physicians with robust tools for data-based decision-making – could all contribute to greater efficiency and cost control.
“The economics of the current system don’t work,” acknowledges Calvin Mitchell, SWHR Vice President of Network Performance. “Healthcare is too expensive. Our population is aging. Medicare is not sustainably funded. Population health strategies increase the efficiency of care, improving outcomes at reduced expense. SWHR assists the provider network with population health strategies in many ways – everything from payor contracts that incentivize quality over volume to population health consultant services. SWHR has a long history of focusing on outcomes. And while we are generally graded by performance in contracts, our actual mission is and should continue to be outcomes and improving people’s lives.”
The need for a fourth and fifth aim
As the burnout of healthcare providers reached a tipping point – exhaustion, professional dissatisfaction and cynicism all contributing – it became evident the healthcare system could not be transformed without addressing the work life-balance of physicians, nurses and other care team members who were weighed down by unrealistic demands, administrative burdens and growing bureaucracy.
“Adding the fourth aim addressing clinician well-being makes sense,” says Jacqueline Mutz, SWHR VP of Care Transformation and Innovation, “because a healthcare system, whether local or national, must have competent and engaged providers across the continuum of care. Good healthcare is dependent upon human beings. If those individuals are suffering from burnout, fatigue or the feeling of being undervalued, it’s harder to come to work focused or with a caring, compassionate attitude.”
Subsequently, a fifth aim was added to the model – advancing health equity – when deep-seated inequities in care became evident due to the coronavirus pandemic. As far back as 1946, the World Health Organization (WHO) Constitution declared that healthcare was a fundamental human right, recognizing “a legal obligation … to ensure access to timely, acceptable and affordable healthcare” for all. The global health crisis precipitated by COVID-19 demonstrated how dramatically our country’s care system had missed the mark.
“Whether it’s due to age, race, religion, sexual identity or geographical location, the ripple effect of not providing equitable access or acceptance for all populations is a continuation of preventable acute, chronic and terminal events and/or diseases that could otherwise be managed,” adds Mutz.
Workforce trends are mixed
In April 2022, David Auerbach, MD, and colleagues published a nursing workforce analysis in Health Affairs, which found the total supply of RNs decreased by more than 100,000 from 2020 to 2021 – the largest single decline ever observed over the previous four decades. A significant number of nurses departing the workforce were under the age of 35, and many were employed in hospitals, creating a severe shortage in nursing. Statewide initiatives are addressing the issue with nursing schools forming strategic partnerships to expand student capacity.
The state of affairs for the physician workforce is more optimistic. Applications to medical school increased by a recording setting 17.8% for the 2021-22 school year, according to the Association of American Medical Colleges (AAMC). This growth has been led by historic increases among underrepresented minorities, a statistic that bodes well for the quintuple aim’s goals of both supporting care teams and improving health equity.
As Southwestern Health Resources strengthens its collaborations with 7,000+ providers across North Texas, the quintuple aim continues to provide a framework for how the clinically integrated network can build a better way to care, together. Fifteen years after introduction of the original triple aim, it is now widely accepted that pursuing each aim together is essential to achieving progress on all of them.
1According to the Peter G. Peterson Foundation, in 2022, the United States spent an estimated $12,555 per person on healthcare — the highest healthcare costs per capita across the 38 countries who make up the Organization for Economic Cooperation and Development (OECD). For comparison, Switzerland was the second highest-spending country with about $8,049 in healthcare costs per capita, while the average for wealthy OECD countries, excluding the US, was only $6,414 per person. Despite higher spending, the United States performs worse in common health metrics like life expectancy, infant mortality and unmanaged diabetes.
2Total cost of care (TCOC) generally refers to direct and indirect costs associated with an episode of care for a period of healthcare coverage (e.g., a health plan’s benefit year).
The statements contained in this article are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this article.



